Five Questions on Breast Cancer Prevention
Author

Suniti Nimbkar, MD
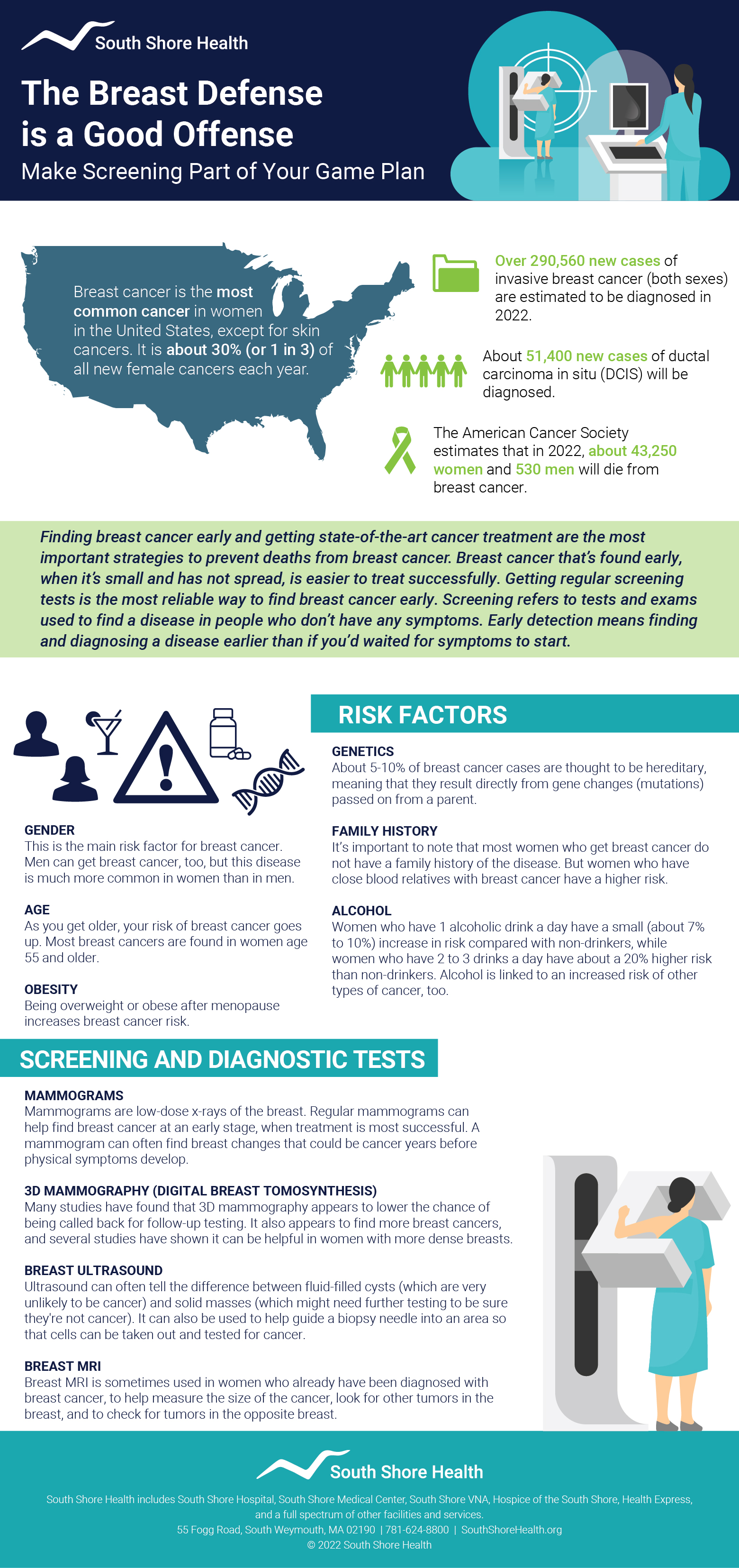
October is Breast Cancer Awareness month. The pink ribbons we see widely displayed on products in stores and supermarkets are a colorful reminder of the disease that affects one in eight American women. It’s also an opportune time to spread awareness about the importance of screening and prevention.
Breast cancer is the second most common cancer in women in the U.S (after skin cancers), and the second leading cause of cancer death in woman (after lung cancer). According to the American Cancer Society, about 287,850 women will be diagnosed with breast cancer in 2022 and 43,250 will die from the disease.
Finding breast cancer early before it has spread is key to successfully treating the disease, which is why I stress the importance of breast cancer screening - including annual mammograms.
Here are five common breast cancer questions I cover with patients.
When it comes to breast cancer prevention, how important are routine or annual screenings?
It is important to recognize that breast cancer screening (mammography) does not prevent breast cancer. The role of screening is to detect cancer early when it is easier to treat.
When we identify very early cancers on mammography, women tend to have better treatment options and an overall excellent prognosis.
In fact, due to the widespread availability of screening mammography in our region, the majority of breast cancers that we identify are in very early stages and treatment outcomes are very favorable.
What kind of screening is available for breast cancer and at what age should people start being screened?
Mammography is the best tool for breast cancer screening.
For a woman at average risk, screening should begin at age 40 and continue annually until age 75. At 75, some women have other significant medical issues that are their primary health concerns.
At this point, a discussion is encouraged between a woman and her primary care doctor to decide if there is a role for ongoing screening.
If a woman is determined to be at high risk for breast cancer, she should have a “Risk Assessment” at a dedicated breast center and screening recommendations will be individualized for her.
What are some of the risk factors for breast cancer and are there lifestyle or diet changes that can lower someone’s risk?
There are modifiable and non-modifiable risk factors for breast cancer; things that we can affect and things we cannot change.
Non-modifiable risk factors:
- Being a woman
- Aging
- Family history
- Previous history of having had a breast biopsy
- Early age of first period
- Late age of menopause
- Never bearing a child
Potentially modifiable risk factors:
- Trying to complete your first pregnancy by age 30
- Breastfeeding
Modifiable risk factors:
- Avoid smoking
- Maintain a healthy body mass index (BMI)
- Exercise 150 minutes a week
- Eat a diet low in red meat/ processed food and high in vegetables, whole grains, fruit, and lean meats (a Mediterranean diet)
- Limit alcohol consumption to no more than three drinks per week
What are some of the symptoms of breast cancer that someone should be concerned about and discuss with their primary care provider or specialist?
The American Cancer Society no longer recommends self-breast exams, but it does advocate for self-breast awareness.
This means that a person should have a sense of what their breasts are like at a baseline and if there are changes, they should report them to their primary care doctor.
Changes could include feeling a lump in the breast or armpit, a change in the size of the breast, nipple changes, redness, or skin changes.
Remember we have two breasts, so it is always a good idea to look at both breasts and if there is a change in one that is not mirrored in the other, have it checked out.
What kind of treatment options are available for someone diagnosed with breast cancer?
The treatment options for breast cancer are extremely focused to the individual patient and the unique features of the cancer. Therefore, it is critically important to have a team approach to breast cancer care.
Patients who are diagnosed with cancer have a team of at least three physicians – a medical oncologist, a surgical oncologist, and a radiation oncologist. This team of three works with the individual patient to create a unique care plan.
Suniti Nimbkar, MD is a Breast Surgical Oncologist and Medical Director of the Breast Care Center at the Dana-Farber Brigham Cancer Center at South Shore Health. Learn more about Breast Care at South Shore Hospital.
Author

Suniti Nimbkar, MD